The Department of laboratory diagnostics performes medical – laboratoric diagnostics in the field of medical biochemistry, laboratoric hematology and coagulation, and cytogenetic diagnosis.
Laboratory program provides more than 200 various search of blood, CSF, urine, secretions, limbs and bowel movement that are manufactured with modern methods, modern technology on modern instruments in order to meet all the requirements of good laboratory practice.
The Department of medical genetics cytogenetic analysis performes on the culture of cells from peripheral blood and amniotic fluid. Laboratory is currently able to provide diagnostic services to determine the karyotype from peripheral blood cell karyotype from amniotic fluid and chorionic villi (prenatal diagnosis).
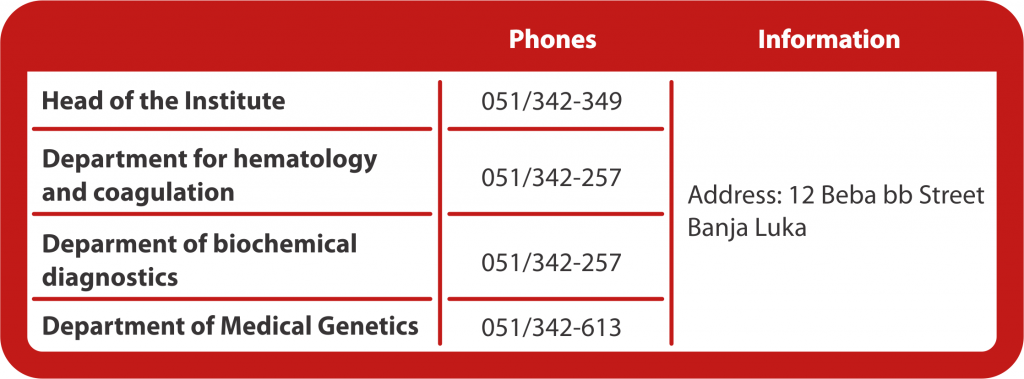
Department consists of three divisions :
1st Department for hematology and coagulation
2nd Department of biochemical diagnostics and
3rd Department of medical genetics
In the first half of 2008, it was launched the process of preparation for the introduction of ISO standards for all laboratory analysis.
General guidelines for patiens in the clinic
In the Institute for laboratoric diagnostics, patients, who are in the clinic, can perform extraction of blood, and taking biological samples for laboratory results from Monday to Friday, between 7:00 am and 10.00 am with a referral from a specialist.
The results are from 05:00 pm to 07.00 pm.
Preparation of patients prior to blood sampling for laboratory results is an important part of appropriate and rational use of laboratory diagnostics, as otherwise the laboratory findings does not have the desired value.
The most appropriate time for taking the blood tests for laboratory findings is in the morning between 7:00 am and 10.00 am (exceptions are functional tests that are done longer).
PREPARATION BEFORE LABORATORY TESTING
General preparation
Before taking a sample of blood, it is not allowed for the patient to eat anything for 12 hours (water is allowed to drink). The day before going to the laboratory is necessary to avoid strong physical effort and taking alcohol.
It is necessary to avoid all medication 48 hours before taking the blood, except that the doctor ordered as required.
Special preparation
Determination of fat in the blood
A patient must be with an empty stomach for 12 hours, and 24 hours before taking the blood must eat light, lean food (do not take milk and milk products, fried foods, eggs, fatty meat, white bread, fat, sweets).
48 hours before taking blood, it is neccessary to avoid hard physical effort and taking alcohol.
Determination of iron in the blood
From the patients who are in the treatment of iron, blood is taken 10 days after peroral, 3 days after intravenous and a month after intramuscular iron preparations.
It is necessary to avoid all medication 48 hours before taking a sample, (except for those who were determined as a doctor required). 24 to 48 hours before going into the laboratory it is not allowed to drink juice enriched with vitamins and blackberry wine.
Implementation of test of oral glucose tolerance (OGTTT)
Test begins between 7 and 8 pm in the morning , and the patient must be with an empty stomach for 12 hours before removing. Three days earlier, the patient is on a normal diet enriched with carbohydrate (bread, pasta, potatoes, rice). During the test, which lasts for 2 hours, the patient must not smoke, eat and drink coffee or other drinks, nor exhibit hard physical activities.
Determination of blood in bowel movement
For seven days before the start of and during the test, it is not alowed to take Andol, aspirin and other painkillers (non-steroidal anti-drug) or iron preparations. Three days before the start of the test
• It is forbidden to eat: liver products (pate, sausages), underdone red meat, white turnip, horse-radish, melon, watermelon, bananas, tomatoes, vitamin C, oranges and lemons.
• It is allowed to eat: well boiled meat, poultry, fish, yogurt, milk, cereals, boiled fruits and vegetables, salads, nuts and peanuts.
The test should be postponed while having diarrhea, menstrual periods, bleeding from hemerrhoids and urinary tract.
Collecting single portions of urine
It is recommended not to urinate 4-8 hours before collecting the sample. Urine should be collected in a clean, washed, dry and wide container. It is not recommended for women to analyse urine right before, during and right after menstruation. After the morning washing of private parts and before breakfast and other activities, the first morning steam of urine should be urinated in the toilet, and the medium is collected in a clean container.
Collecting urine for 24 hours
Collection of urine starts with the second morning urine since the first one is urinated in the toilet. Furthermore, during the whole day and night sould be urinated into one or more containers, and the next morning, the first morning urine sould be added. Containers (plastic bottles are most suitable) must be previously well washed, and collected urine should be kept in a cool place. For the analysis of uric acid and ammonia in the urine, it is necessary to ask for a preservative, from the laboratory staff, that is put into containers for collecting urine.
Taking blood
Taking blood from a finger
It is recommended taking blood from the ring-finger of the left hand (to the left-handed persons blood should be taken from right hand), and children- from the middle finger. Previously, hands shold be warm for better blood circulation. With strong and short stabs, with lancet, on the previously desinfected surface, the first drop of blood which begins to flow should be deleted, and then collected the following upcoming drops.
Taking venous blood (from the forearm)
For taking blood, one-time sterile needles are used and tubes with a single purpose under pressure. A patient is in a sitting position, frees one hand, squeeze hand, and a laboratory technician allows easier access to vein, with a suspender. After taking the blood, it is important that the patient keeps his hand extended for 5 minutes and with the second hand to press cotton pad in place of sting.

 Standard procedure for work of the ethical committee of the clinical center (kc)
Standard procedure for work of the ethical committee of the clinical center (kc)